With the increased interest in the GLP-1 agonist category of medications, I decided to introduce everyone to GLP-1 and explain how it works. Before we begin, remember that a GLP-1 agonist is not GLP-1, nor does it support the body’s natural production of GLP-1. An agonist is a drug or substance that binds to a receptor inside a cell or on its surface and causes the same action as the substance that normally binds to the receptor. Ideally, it would be best if we could support the body’s production of GLP-1 and support the much-needed benefits you will learn about below.
What is GLP-1?
GLP-1 stands for Glucagon-like peptide-1 (GLP-1). It is an incretin hormone that plays a crucial role in glucose metabolism and other physiological processes. The gut releases an incretin hormone in response to food intake, particularly when carbohydrates and fats enter the small intestine. Incretin hormones play a crucial role in regulating glucose metabolism by enhancing insulin secretion from the pancreas after eating before blood glucose levels rise significantly. They help the body efficiently manage postprandial (after eating) blood sugar levels.
The Two Main Incretin Hormones[i]
- GLP-1: Released by the L-cells of the small intestine, GLP-1 stimulates insulin secretion, inhibits glucagon release (a hormone that raises blood glucose), slows gastric emptying, and promotes satiety, helping to control appetite.
- Gastric inhibitory polypeptide (GIP): Released by K-cells in the small intestine, GIP also stimulates insulin secretion. However, unlike GLP-1, it does not inhibit glucagon secretion or slow gastric emptying.
Primary Functions of Incretins[ii]:
- Enhance insulin secretion: They act on the pancreatic β-cells to increase insulin release in response to food.
- Suppress glucagon secretion: They reduce the release of glucagon, which helps lower the liver’s glucose production.
- Modulate gastric emptying: Slowing the rate at which food leaves the stomach helps regulate post-meal blood sugar levels.
- Promote satiety: By interacting with receptors in the brain, incretin hormones help reduce appetite and food intake.
What Physiological Processes Does GLP-1 Impact?
Stimulates Insulin Secretion (Incretin Effect)[iii]
GLP-1 is primarily known for enhancing insulin secretion in response to nutrient intake, mainly carbohydrates. It acts on pancreatic β-cells to increase insulin release, thereby lowering blood glucose levels in a glucose-dependent manner.
Suppresses Glucagon Secretion[iv]
GLP-1 also inhibits glucagon release from pancreatic α-cells. Glucagon normally raises blood glucose levels by stimulating the liver to produce glucose. By suppressing glucagon, GLP-1 helps reduce hepatic glucose output.
Slows Gastric Emptying[v]
GLP-1 slows gastric emptying, which prolongs the digestion process and helps to reduce postprandial blood glucose spikes. This action promotes satiety and aids in the regulation of appetite.
Promotes Satiety and Reduces Appetite[vi]
GLP-1 acts on the central nervous system (CNS), particularly in the hypothalamus, to induce a feeling of fullness (satiety).
Improves β-Cell Function and Proliferation[vii]
GLP-1 has a trophic effect on pancreatic β-cells. It promotes β-cell proliferation, inhibits β-cell apoptosis, and enhances insulin gene expression, which can improve pancreatic function over time.
Cardioprotective Effects[viii]
GLP-1 has been shown to benefit the cardiovascular system, including improving endothelial function, reducing blood pressure, and exerting anti-inflammatory effects.
Neuroprotective Effects[ix]
Emerging evidence suggests that GLP-1 has neuroprotective effects, including reducing oxidative stress, promoting neuronal survival, and potentially improving cognitive function. These findings are particularly relevant to the study of neurodegenerative conditions.
GLP-1 Agonist vs. GLP-1 Natural Production
GLP-1 Agonists
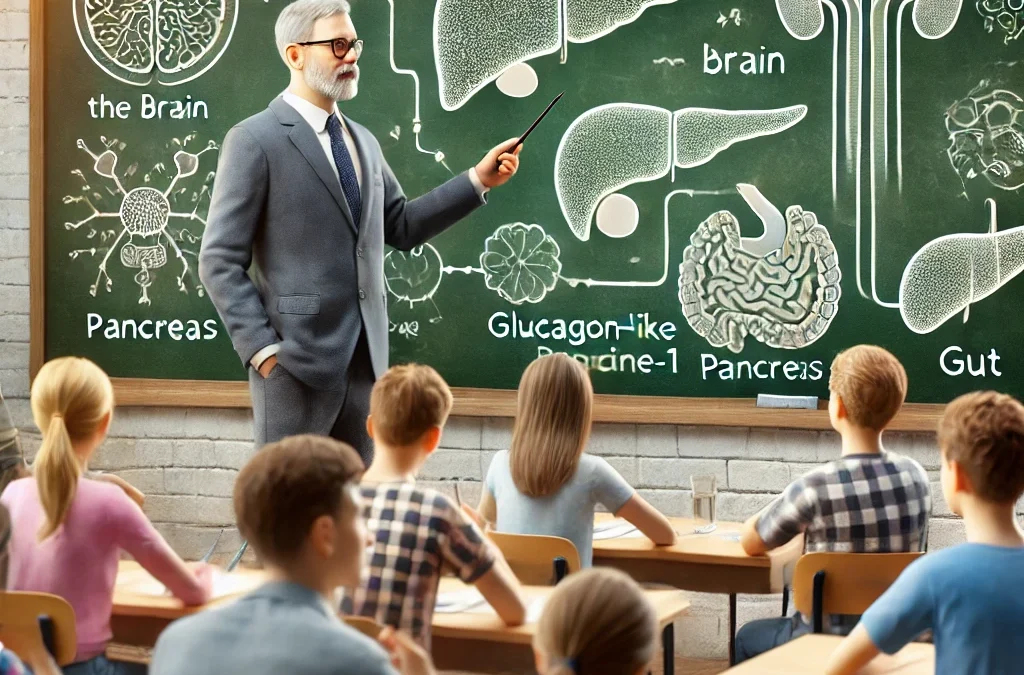
A GLP-1 agonist (GLP1-A) is a drug or substance that binds to receptors in three areas of the body: Brain, Pancreas, and Gastrointestinal Tract[x].
- In the brain, GLP-1 As activates GLP-1 receptors in the hypothalamus, which regulates food intake. This decreases the feeling of hunger and increases satiety.
- In the pancreas, GLP-1As activate GLP-1 receptors, which increase insulin release and reduce glucagon release.[xi]
- In the gut, GLP-1 is used to slow stomach emptying. This makes you feel full longer.[xii]
GLP-1 agonist drugs provide much higher levels of GLP-1 receptor agonism than GLP-1, which is naturally produced by the body. This could be why these medications are triggering gastrointestinal side effects.[xiii]
Supporting GLP-1 Natural Production
To best understand the difference, we must look at the definition of supporting the body.
In medicine, “supporting the body” refers to a treatment approach that aims to assist the body’s natural healing mechanisms by providing necessary support and interventions that work with the body’s physiology, while “forcing the body” implies interventions that aggressively push the body beyond its natural limits, potentially causing harm by overriding its inherent processes; essentially, it’s the difference between working with the body’s natural abilities to heal and actively trying to manipulate it against its will. Forcing often leads to unwanted side effects and imbalance (not homeostasis).
Examples:
Supporting the body:
A doctor recommends dietary changes and exercise for someone with high blood pressure rather than immediately prescribing medication.
Forcing the body:
Administering a very high dose of a medication to quickly alleviate symptoms, even if it means significant side effects.
Supporting the body’s natural production of GLP-1 is quite different than giving the body a “drug” version. GLP-1 agonists are not GLP-1 but a modified version of GLP-1 that is more active on a receptor. Natural GLP-1 is broken down quickly (the body’s natural process) versus GLP-1 agonists, which are designed to resist being broken down (allowing them to stay in the bloodstream longer).[xiv]
Supporting the body’s natural production of GLP-1 provides the same benefits as a GLP-1 agonist in the brain, pancreas, and gut. Still, it is the natural form of GLP-1 and not a chemical entity that mimics GLP-1. In an ideal situation, the goal would be to seek natural alternatives to help support the body’s natural production of GLP-1 and avoid the potential for undesirable side effects. The body’s production of GLP-1 is influenced by the nutrients.
Conclusion
The emergence of GLP-1 agonists and their physiological benefits have opened the door to increased research and development of what may support the body’s production of GLP-1 instead of providing a mimicker (agonist). Stay tuned for what I find!
[i] Drucker DJ. The biology of incretin hormones. Cell Metab. 2006 Mar;3(3):153-65. doi: 10.1016/j.cmet.2006.01.004. PMID: 16517403.
[ii] Drucker DJ. The biology of incretin hormones. Cell Metab. 2006 Mar;3(3):153-65. doi: 10.1016/j.cmet.2006.01.004. PMID: 16517403.
[iii] Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007 Oct;87(4):1409-39. doi: 10.1152/physrev.00034.2006. PMID: 17928588.
[iv] Nauck MA, Heimesaat MM, Orskov C, Holst JJ, Ebert R, Creutzfeldt W. Preserved incretin activity of glucagon-like peptide 1 [7-36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J Clin Invest. 1993 Jan;91(1):301-7. doi: 10.1172/JCI116186. PMID: 8423228; PMCID: PMC330027.
[v] Maselli DB, Camilleri M. Effects of GLP-1 and Its Analogs on Gastric Physiology in Diabetes Mellitus and Obesity. Adv Exp Med Biol. 2021;1307:171-192. doi: 10.1007/5584_2020_496. PMID: 32077010.
[vi] Flint A, Raben A, Astrup A, Holst JJ. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J Clin Invest. 1998 Feb 1;101(3):515-20. doi: 10.1172/JCI990. PMID: 9449682; PMCID: PMC508592.
[vii] Maselli DB, Camilleri M. Effects of GLP-1 and Its Analogs on Gastric Physiology in Diabetes Mellitus and Obesity. Adv Exp Med Biol. 2021;1307:171-192. doi: 10.1007/5584_2020_496. PMID: 32077010.
[viii] Ussher JR, Drucker DJ. Cardiovascular biology of the incretin system. Endocr Rev. 2012 Apr;33(2):187-215. doi: 10.1210/er.2011-1052. Epub 2012 Feb 8. PMID: 22323472; PMCID: PMC3528785.
[ix] Erbil D, Eren CY, Demirel C, Küçüker MU, Solaroğlu I, Eser HY. GLP-1’s role in neuroprotection: a systematic review. Brain Inj. 2019;33(6):734-819. doi: 10.1080/02699052.2019.1587000. Epub 2019 Apr 2. PMID: 30938196.
[x] Shaefer CF Jr, Kushner P, Aguilar R. User’s guide to mechanism of action and clinical use of GLP-1 receptor agonists. Postgrad Med. 2015;127(8):818-26. doi: 10.1080/00325481.2015.1090295. Epub 2015 Sep 15. PMID: 26371721.
[xi] Shaefer CF Jr, Kushner P, Aguilar R. User’s guide to mechanism of action and clinical use of GLP-1 receptor agonists. Postgrad Med. 2015;127(8):818-26. doi: 10.1080/00325481.2015.1090295. Epub 2015 Sep 15. PMID: 26371721.
[xii] Shaefer CF Jr, Kushner P, Aguilar R. User’s guide to mechanism of action and clinical use of GLP-1 receptor agonists. Postgrad Med. 2015;127(8):818-26. doi: 10.1080/00325481.2015.1090295. Epub 2015 Sep 15. PMID: 26371721.
[xiii] Shaefer CF Jr, Kushner P, Aguilar R. User’s guide to mechanism of action and clinical use of GLP-1 receptor agonists. Postgrad Med. 2015;127(8):818-26. doi: 10.1080/00325481.2015.1090295. Epub 2015 Sep 15. PMID: 26371721.
[xiv] Lee S, Lee DY. Glucagon-like peptide-1 and glucagon-like peptide-1 receptor agonists in the treatment of type 2 diabetes. Ann Pediatr Endocrinol Metab. 2017 Mar;22(1):15-26. doi: 10.6065/apem.2017.22.1.15. Epub 2017 Mar 31. PMID: 28443255; PMCID: PMC5401818.